
Molecular Hydrogen and its Application as an Adjunct or hydrogen gas Mono-therapy in Malignant diseases
Compiled and published by KYKSA
Why is cancer so difficult to treat ?
Why does very few people know of or about Hydrogens impact on cancer treatment?
The short answer is that it is a reasonable new discovery (2007) and only really investigated and exploited as adjunct and Mono-therapy for an ever-growing range of Oxidative stress triggered (Why choose Molecular Hydrogen) diseases since 2010. With the stringent nature of publications of research articles in leading international journals, (it is a 3 to 5 year process) of research, review and publication. No wonder it is reasonable unknown.
Advanced cancer treatment is a huge challenge and new strategies and treatments are required.
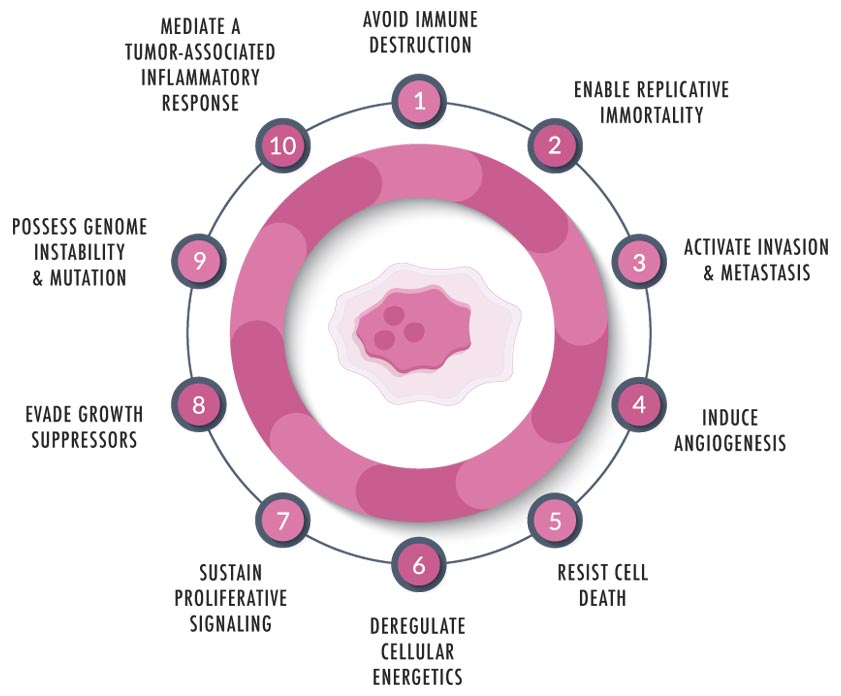
Oxidative stress is involved in cancer development and progression. Hydrogen-gas (H2) is the most powerful, novel and the only SELECTIVE antioxidant. It exhibits strong anti-inflammatory and anti-cancer activities. What is Hydrogen-Gas (H2) and the Science behind it?
Hydrogen is a natural, colourless, odourless, MEDICAL gas. The potent antioxidant potential was discovered by the Japanese Professor, Dr Shigeo Otha (PHD) and published in the most prestigious journals ?NATURE MEDICINE? and ?SCIENCE?. This has gained the attention from academic researchers, medical doctors, and physicians around the world. Hydrogen Gas in Cancer Treatment
Since the discovery by Dr Otha, more than 1600 researchers have teamed up globally in the biomedical research of hydrogen. These scientific publications have also conclusively demonstrated that hydrogen-gas provides therapeutic potential in the prevention and treatment of cancers.
In December 2019, hydrogen-gas therapy has now for the first time demonstrated to be also effective in the treatment of brain metastases after conventional treatments failed. This is significant and exiting as standard chemotherapy is ineffective because of the blood?brain barrier. Due to its unique size, hydrogen gas can cross the blood-brain-barrier and penetrate ALL body cells.
Case Study
?A 44-year-old woman diagnosed with lung cancer with multiple metastases in November 2015. Oral targeted drugs were initiated after the removal of brain metastases, and most lesions remained stable for 28 months. In March 2018, intracranial multiple metastases, as well as hydrocephalus accumulation in the third ventricle and lateral ventricles, and metastases in bone, adrenal gland, liver were noted. Hydrogen-gas monotherapy was started to control the tumour a month later. After 4 months, the size of multiple brain tumours was reduced significantly, and the amount of hydrocephalus in the third ventricle and lateral ventricles reduced significantly. After 1 year, all brain tumours had disappeared, and there were no significant changes in metastases in the liver and lung. These data show that, after standard treatments had failed, hydrogen-gas monotherapy elicited significant effective control of tumours (especially those in the brain) ?
? Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6927257/
?Hydrogen Gas Suppresses Tumour Formation
?Hydrogen Gas Suppresses Tumour Growth
?Hydrogen Gas Prevents/Relieves the Harmful Side Effects Related to Chemotherapy and Radiotherapy
Hydrogen Gas in Cancer Treatment
So far, over 1000 high quality scientific studies have demonstrated that hydrogen-gas provides therapeutic potential for the prevention and treatment of more than 170 human and animal disease models including cancers, diabetes and heart disease.
The clinical and pre-clinical studies demonstrate that hydrogen-gas is providing antioxidant, anti-tumour, anti-inflammatory, anti-diabetes, anti-allergy, anti-obesity and anti-apoptosis properties.
Hydrogen-gas reduces oxidative stress and improves redox homeostasis partly mediated via the Nrf2 pathway, which regulates levels of glutathione, superoxide dismutase, catalase, etc.
Is Hydrogen Gas Safe?
Absolutely! The FDA and the clinical papers validate that hydrogen-gas is 100% safe, has no side-effects whatsoever, can never be overdosed and is even safe and beneficial for pregnant woman and babies. Hydrogen-gas is NOT a foreign substance, but it is natural to the human body. During our best years, our gut bacteria is able to produce litres of hydrogen-gas after a fibre rich meal. However, as we get older, this process slows down. This is linked to the aging process and the development of over 90% of all diseases. Hydrogen-gas will provide the body with the important SELECTIVE antioxidants to eliminate HARMFUL FREE RADICALS which are responsible for the aging process and disease development.
The Japanese government has recently approved hydrogen-gas inhalation as an advanced medicine?

How to get your Daily Dose of Hydrogen-Gas?
There are several effective delivery methods. Hydrogen-gas can be administered via direct inhalation of the therapeutic gas. This method is preferred for patients suffering from cancers and was used in most pre-clinical and clinical studies. It provides highest hydrogen-gas concentration and organ saturation. The ability to directly inhale the gas provides an easy to administer, comfortable and affordable treatment option. The treatment does not require certification and can be administered by the patients in the comfort of their homes.
No nursing staff is required. Hydrogen Gas in Cancer Treatment
Brain Metastases Completely Disappear in Non-Small Cell Lung Cancer Using Hydrogen Gas Inhalation: A Case Report
Jibing Chen,1 Feng Mu,1 Tianyu Lu,1 Duanming Du,2 and Kecheng Xu1
Author information Article notes Copyright and License information Disclaimer
This article has been cited by other articles in PMC.
Abstract
Introduction
Non-small-cell lung cancer (NSCLC) is the second most frequently diagnosed tumour worldwide, and is the leading cause of cancer-related deaths.1 With respect to metastasis of NSCLC, there are some preferential sites (bone, 34.3%; lung, 32.1%; brain, 28.4%; adrenal glands, 16.7%; liver,
13.4%).2 NSCLC metastasizes to the brain in 10?25% of all cases. This type of spread can lead to significant morbidity and mortality, and 5-year survival has been reported to be 3.6%.3 No significant changes in 5-year survival for patients with NSCLC metastases to the brain have been observed in the last three decades.1,4 The short-term survival of NSCLC patients with brain metastases is due to the lack of efficacious therapies. Standard chemotherapy is ineffective because of the blood?brain barrier. Radiotherapy and neurosurgery are recognized as locoregional methods;5 molecularly targeted therapies and immunotherapies are recognized as systemic treatments.6
In 2018, Wang et al7 reported on delivery of different concentrations of hydrogen gas into two culture systems for lung cancer cells (A549 and H1975). They found that the ability of cells to divide, migrate and infiltrate into tissue was inhibited significantly, and that apoptosis was accelerated. Also, lung cancer tumour-bearing mice were treated with hydrogen gas for 4 weeks, and the tumour volume was reduced by 25%. The reason for these phenomena was that hydrogen can reduce the expression of structural maintenance of chromosomes 3 (SMC3), SMC5, SMC6 in lung cancer cells.
Also in 2018, Akagi and Baba8 reported the results of hydrogen gas monotherapy for patients with stage-IV colon cancer. They found that the proportion of programmed death (PD)-1+CD8+ T-cell subsets in the blood of patients was reduced upon continuous inhalation of hydrogen, and was reduced by ~60% after several months. After 3 years of follow-up, progression-free survival and overall survival were prolonged significantly.
Here, we report a 44-year-old woman diagnosed with NSCLC and multiple metastases. After resection of an intracranial metastasis and targeted drug therapy, the outcome was good, but NSCLC metastasized (brain, cerebellum, lung, liver, bones and adrenal glands) after 28 months of treatment. In view of the literature stated above, she underwent hydrogen inhalation, and brain metastases disappeared after 4 months. Intracranial recurrence was not found after 1 year of treatment, and other metastatic sites remained stable.
Case Presentation
In November 2015, a 44-year-old woman was admitted to our hospital complaining of dizziness and instability upon standing. Through chest computed tomography (CT) and cranial magnetic resonance imaging (MRI) examination, we found multiple tumours in the left cranial cavity and right lung. After resection of an intracranial tumour, pathology studies suggested metastatic lung adenocarcinoma. Genetic testing suggested mutation of the epidermal growth factor receptor (EGFR) gene at exon 19. She started taking gefitinib tablets (Iressa?, 250 mg, once daily). The intracranial and lung tumours were controlled well until June 2017 (Figure 1).
Figure 1
Post-contrast brain MR Imaging of the head before and after treatment. In November 2015, the patient was found to have lung cancer with brain (left, 4.4�3.1 cm) and cerebellar (right, 4.0�3.1 cm) metastasis. After resection and targeted drug therapy, there was no recurrence of metastases after 19 months. Solid arrow = brain metastasis; hollow arrow = cerebellar metastasis.
When a review was conducted in September 2017, the disease had progressed. A combination of pemetrexed and erlotinib was initiated, and the tumours were controlled again. The intracranial and lung tumours progressed again in March 2018, and the targeted treatment regimen was adjusted to icotinib hydrochloride (125 mg, t.d.s.).
After 2 weeks, the patient suddenly complained of dyspnea, and difficulties in speaking. Enhanced MR imaging of the head revealed multiple nodular metastases in the left cranial cavity; the third ventricle and lateral ventricles accumulated hydrocephalus, and the largest lesion was in the frontal lobe (1.9 � 1.4 cm) (Figure 2A). Computed tomography showed that the lesion on the upper lobe of the right lung was enlarged (1.2 � 0.6 cm), and new metastases were found at the lower lobe of the right lung, mediastinum, lung hilum (1.7 � 1 cm), seventh thoracic spine and left adrenal gland. The patient refused radiotherapy and surgery of brain, signed informed consent of hydrogen therapy and agreed on the publication of the case.
Figure 2
Post-contrast brain MRI of the head before and after hydrogen inhalation. (A) In April 2018, the patient was found to have multiple metastases (white arrows) in the brain (left, 2.5�3.0 cm and 2.4�2.8 cm for two bigger tumours) and cerebellum (right, 1.3�1.8 cm and 1.2�0.7 cm for two bigger tumours). Also, the third ventricle and lateral ventricles were expanded and had accumulated hydrocephalus. (B) After 4 months of hydrogen inhalation, all tumours visible to the naked eye had disappeared, and the shape of ventricles had returned to normal. (C) After 1 year of inhalation (April 2019), recurrence had not occurred.
From April 2018, the patient began hydrogen inhalation and received no other treatments during the time period. The hydrogen oxygen nebulizer (AMS-H-03, Asclepius Meditec, Shanghai, China) generates 3 L/min hydrogen gas by hydrocephalus electrolysis. As measured by gas chromatography, the gas generated consisted of 67% hydrogen and 33% oxygen. Using a special mask, the patient continued to inhale hydrogen for 3?6 hrs a day at rest, with no interruption even after the obvious relief of symptoms. After 4 months, most brain metastases disappeared and the amount of hydrocephalus in the third ventricle and lateral ventricles were both reduced (Figure 2B). After 1 year, all visible brain tumours had disappeared, and there were no obvious changes in metastases in the liver and lung (Figure 2C).
There were increased levels of carcinoembryonic antigen (CEA, 29.44 ng/mL), carbohydrate antigen-125 (CA125, 153 U/mL) and cytokeratin fragment antigen21-1 (CYFRA21-1, 12.1 ng/mL) before the patient started hydrogen monotherapy. Serum levels of these three markers continued to decrease after 4 months of treatment (21.6 ng/mL, 83 U/mL and 8.5 ng/mL, respectively), and were close to (but remained above) the reference range after 1 year of treatment (12.3 ng/mL, 61 U/mL and 5.9 ng/mL, respectively) (Figure 3).
Figure 3
Detection of serum tumour markers before and after hydrogen inhalation. The red line and the lower area in each figure represent the normal range.
Abbreviations: CEA, carcinoembryonic antigen; CA125, carbohydrate antigen 125; CYFRA21-1, cytokeratin fragment antigen 21?1.
Discussion
In general, NSCLC cells tend to metastasize to the brain, bones and adrenal glands, adenocarcinomas metastasize to the brain, and squamous cell carcinomas metastasize to bones. The exact homing mechanisms and how cancer cells communicate with this new stroma are not known.
Brain metastasis of NSCLC cells is closely related to various signalling pathways, several of which involve the participation of hydrogen gas. In 2013, Bleckmann et al9 reported that, within the Wnt pathway, T-cell factor (TCF)/lymphoid enhancer factor (LEF-1) act independently of ?-catenin in human lung adenocarcinomas that metastasize to the cerebrum. In 2014, Kafka et al10 reported altered expression of dishevelled (DVL)-1, DVL-3, E-cadherin, and ?-catenin in brain metastases of adenocarcinomas, which again suggested the importance of Wnt signalling. Lin et al11 were the first (in 2016) to demonstrate that hydrogen gas suppresses abnormal activation of Wnt/?-catenin signalling.
Crosstalk between EGFR and MET, the hepatocyte growth factor (HGF) receptor, has been reported in adenocarcinomas that have metastasized to the brain. This is not a direct interaction but instead signalling via activation of mitogen-activated protein kinases (MAPKs).12 In 2017, Yang et al13 found that hydrogen-containing saline can decrease phosphorylation of p38 MAPK and Smad2/3 in a rat model of cardiac fibrosis. In 2019, Guan et al14 reported that hydrogen gas can ameliorate chronic intermittent hypoxia-induced kidney injury by inhibiting oxidative stress-dependent activation of p38 and c-Jun N-terminal kinase (JNK). Similar results were demonstrated by Zhang and colleagues in experiments on the proliferation and migration of vascular smooth muscle cells.15 Han et al showed that sirtuin (SIRT)1 is highly expressed in brain metastasis,16 and several scholars have demonstrated that hydrogen can suppress SIRT1 signalling in different models.17?19 Those studies suggest that hydrogen gas has a unique therapeutic effect on the brain metastasis of NSCLC.
Several interesting studies have focused on the comparison of genomic alterations between primary lung carcinomas versus metastases to the brain and bone. The hypothesis is that there might be clonal diversity between these two. In our patient, there was a considerable difference between brain metastasis and other extrapulmonary metastases. This was most likely due to the clonal diversity of different metastatic sites, which resulted in significant differences in sensitivity to hydrogen inhalation.
As with many biomarker studies focusing on single genes/proteins, a selection bias or overinterpretation can occur. Shen et al20 found higher levels of metastasis-associated lung adenocarcinoma transcript-1 (MALAT1) in brain metastases compared with those in other extrapulmonary sites. A similar investigation searched for brain-metastasis genes and discovered a regulator of epithelial?mesenchymal transition (EMT); pre-B cell leukaemia homeobox (PBX)-regulating protein-1 (PREP1) overexpression triggered EMT, whereas PREP1 downregulation inhibited EMT induction in response to transforming growth factor-? expression. PREP1 modulates sensitivity to SMAD3 and induces expression of Fos-related antigen (FRA)-1. FRA-1 and PBX1 are required for the mesenchymal changes triggered by PREP1 in lung tumour cells. PREP1-induced EMT correlates with increased lung colonization, and PREP1 accumulation has been found in human brain metastases.21 When investigating adenocarcinomas with rearrangement of activin receptor-like
kinase, amplification of the fibroblast growth factor receptor (FGFR)1 gene correlated significantly with brain metastases. Although in those cases there were more visceral metastases, FGFR1 amplification in the brain metastases of adenocarcinomas were fivefold more frequent than that in the primary tumors.22
Also, C-X-C motif chemokine receptor (CXCR)4 seems to have a role in brain metastasis. CXCR4 protein has been shown to be highly overexpressed in patients with brain-specific metastasis but significantly less in NSCLC patients with metastases to other organs and in patients without metastases.23 Also, a disintegrin and metallopeptidase domain 9 (ADAM9) expression have been reported to be relatively higher in brain metastases than that in primary lung tumours. ADAM9 regulates metastasis of lung cancer cells to the brain by facilitating tissue plasminogen activator-mediated cleavage of CUB domain-containing protein-1.24
We are the first to report the efficacy of hydrogen on brain metastases from NSCLC. Our patient has survived for >1 year with hydrogen inhalation, and indicators such as serum tumour markers are improving continuously. We explored the possible reason for hydrogen to inhibited NSCLC brain metastasis in this patient (e.g. TCF/LEF-1 and DVL-1/3 of Wnt/?-catenin signalling, MAPK, and SIRT1), and proposed differences in the expression of signalling molecules between brain metastasis and other extrapulmonary metastases (e.g. MALAT1, EMT, PREP1, FGFR1, CXCR4 and ADAM9).
Conclusions
Hydrogen inhalation may have had a role in the treatment of our patient in different ways.
For example, hydrogen exerts neuroprotective effects by reducing cyclooxygenase-2 activity25 or activating expression of anti-apoptotic protein kinase B.26 Also, hydrogen can inhibit expression of pro-apoptotic factors such as JNK and caspase-3.25,27 Hydrogen inhalation can down-regulate the expression of various pro-inflammatory cytokines, including interleukin (IL)-1?, IL-6, tumour necrosis factor-?, intracellular adhesion molecule-1, high mobility group box-1, nuclear factor-kappa B, and prostaglandin-E2.28 Whether the mechanisms mentioned above are related to the therapeutic effect of hydrogen must be confirmed by further research.
Ethics Approval and Consent for Publication
This research was approved by the research ethics committee of Fuda Cancer Hospital of Jinan University, and written informed consent for publication of the clinical details and images was obtained from the patient.
Author Contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest regarding this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7?34.
doi:10.3322/caac.21551 [PubMed] [CrossRef] [Google Scholar]
2. Tamura T, Kurishima K, Nakazawa K, et al. Specific organ metastases and survival in metastatic non-small-cell lung cancer. Mol Clin Oncol. 2015;3(1):217?221. doi:10.3892/mco.2014.410 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3. Ulahannan D, Khalifa J, Faivre-Finn C, et al. Emerging treatment paradigms for brain metastasis in non-small-cell lung cancer: an overview of the current landscape and challenges ahead. Ann Oncol. 2017;28(12):2923?2931. doi:10.1093/annonc/mdx481 [PubMed] [CrossRef] [Google Scholar]
4. Goldstraw P, Chansky K, Crowley J, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (Eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39?51. doi:10.1016/j.jtho.2015.09.009 [PubMed]
[CrossRef] [Google Scholar]
5. Sperduto PW, Yang TJ, Beal K, et al. Estimating survival in patients with lung cancer and brain metastases: an update of the graded prognostic assessment for lung cancer using molecular markers (lung-molGPA). JAMA Oncol. 2017;3(6):827?831. doi:10.1001/jamaoncol.2016.3834 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
6. Metro G, Chiari R, Ricciuti B, et al. Pharmacotherapeutic options for treating brain metastases in non-small cell lung cancer. Expert Opin Pharmacother. 2015;16(17):2601?2613.
doi:10.1517/14656566.2015.1094056 [PubMed] [CrossRef] [Google Scholar]
7. Wang D, Wang L, Zhang Y, et al. Hydrogen gas inhibits lung cancer progression through targeting SMC3. Biomed Pharmacother. 2018;104:788?797. doi:10.1016/j.biopha.2018.05.055 [PubMed]
[CrossRef] [Google Scholar]
8. Akagi J, Baba H. Hydrogen gas restores exhausted CD8+ T cells in patients with advanced colorectal cancer to improve prognosis. Oncol Rep. 2019;41(1):301?311. doi:10.3892/or.2018.6841 [PubMed] [CrossRef] [Google Scholar]
9. Bleckmann A, Siam L, Klemm F, et al. Nuclear LEF1/TCF4 correlate with poor prognosis but not with nuclear beta-catenin in cerebral metastasis of lung adenocarcinomas. Clin Exp Metastasis. 2013;30(4):471?482. doi:10.1007/s10585-012-9552-7 [PMC free article] [PubMed]
[CrossRef] [Google Scholar]
10. Kafka A, Tomas D, Beros V, et al. Brain metastases from lung cancer show increased expression of DVL1, DVL3 and beta-catenin and down-regulation of E-cadherin. Int J Mol Sci. 2014;15(6):10635?10651. doi:10.3390/ijms150610635 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Lin Y, Ohkawara B, Ito M, et al. Molecular hydrogen suppresses activated Wnt/beta-catenin signaling. Sci Rep. 2016;6:31986. doi:10.1038/srep31986 [PMC free article] [PubMed]
[CrossRef] [Google Scholar]
12. Breindel JL, Haskins JW, Cowell EP, et al. EGF receptor activates MET through MAPK to enhance non-small cell lung carcinoma invasion and brain metastasis. Cancer Res. 2013;73(16):5053?5065. doi:10.1158/0008-5472.CAN-12-3775 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
13. Yang J, Wu S, Zhu L, et al. Hydrogen-containing saline alleviates pressure overload-induced interstitial fibrosis and cardiac dysfunction in rats. Mol Med Rep. 2017;16(2):1771?1778.
doi:10.3892/mmr.2017.6849 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. Guan P, Sun ZM, Luo LF, et al. Hydrogen protects against chronic intermittent hypoxia induced renal dysfunction by promoting autophagy and alleviating apoptosis. Life Sci. 2019;225:46?54.
doi:10.1016/j.lfs.2019.04.005 [PubMed] [CrossRef] [Google Scholar]
15. Zhang YX, Xu JT, You XC, et al. Inhibitory effects of hydrogen on proliferation and migration of vascular smooth muscle cells via down-regulation of mitogen/activated protein kinase and ezrin-radixin-moesin signaling pathways. Chin J Physiol. 2016;59(1):46?55. doi:10.4077/CJP.2016.BAE365 [PubMed] [CrossRef] [Google Scholar]
16. Han L, Liang XH, Chen LX, et al. SIRT1 is highly expressed in brain metastasis tissues of non-small cell lung cancer (NSCLC) and in positive regulation of NSCLC cell migration. Int J Clin Exp Pathol. 2013;6(11):2357?2365. [PMC free article] [PubMed] [Google Scholar]
17. Xing Z, Pan W, Zhang J, et al. Hydrogen rich hydrocephalus attenuates renal injury and fibrosis by regulation transforming growth factor-beta induced Sirt1. Biol Pharm Bull. 2017;40(5):610?615. doi:10.1248/bpb.b16-00832 [PubMed] [CrossRef] [Google Scholar]
18. Sun Q, Han W, Hu H, et al. Hydrogen alleviates hyperoxic acute lung injury related endoplasmic reticulum stress in rats through upregulation of SIRT1. Free Radic Res. 2017;51(6):622?632.
doi:10.1080/10715762.2017.1351027 [PubMed] [CrossRef] [Google Scholar]
19. Li S, Fujino M, Ichimaru N, et al. Molecular hydrogen protects against ischemia-reperfusion injury in a mouse fatty liver model via regulating HO-1 and Sirt1 expression. Sci Rep. 2018;8(1):14019. doi:10.1038/s41598-018-32411-4 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
20. Shen L, Chen L, Wang Y, et al. Long noncoding RNA MALAT1 promotes brain metastasis by inducing epithelial-mesenchymal transition in lung cancer. J Neurooncol. 2015;121(1):101?108. doi:10.1007/s11060-014-1613-0 [PubMed] [CrossRef] [Google Scholar]
21. Li Q, Yang J, Yu Q, et al. Associations between single-nucleotide polymorphisms in the PI3K-PTEN-AKT-mTOR pathway and increased risk of brain metastasis in patients with non-small cell lung cancer. Clin Cancer Res. 2013;19(22):6252?6260. doi:10.1158/1078-0432.CCR-13-1093 [PubMed]
[CrossRef] [Google Scholar]
22. Preusser M, Berghoff AS, Berger W, et al. High rate of FGFR1 amplifications in brain metastases of squamous and non-squamous lung cancer. Lung Cancer. 2014;83(1):83?89.
doi:10.1016/j.lungcan.2013.10.004 [PubMed] [CrossRef] [Google Scholar]
23. Wang L, Wang Z, Liu X, et al. High-level C-X-C chemokine receptor type 4 expression correlates with brain-specific metastasis following complete resection of non-small cell lung cancer. Oncol Lett. 2014;7(6):1871?1876. doi:10.3892/ol.2014.1979 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
24. Lin CY, Chen HJ, Huang CC, et al. ADAM9 promotes lung cancer metastases to brain by a plasminogen activator-based pathway. Cancer Res. 2014;74(18):5229?5243. doi:10.1158/0008-5472.CAN-13-2995 [PubMed] [CrossRef] [Google Scholar]
25. Yang Y, Zhu Y, Xi X. Anti-inflammatory and antitumor action of hydrogen via reactive oxygen species. Oncol Lett. 2018;16(3):2771?2776. doi:10.3892/ol.2018.9023 [PMC free article] [PubMed][CrossRef] [Google Scholar]
26. Hou Z, Luo W, Sun X, et al. Hydrogen-rich saline protects against oxidative damage and cognitive deficits after mild traumatic brain injury. Brain Res Bull. 2012;88(6):560?565.
doi:10.1016/j.brainresbull.2012.06.006 [PubMed] [CrossRef] [Google Scholar]
27. Sun H, Chen L, Zhou W, et al. The protective role of hydrogen-rich saline in experimental liver injury in mice. J Hepatol. 2011;54(3):471?480. doi:10.1016/j.jhep.2010.08.011 [PubMed]
[CrossRef] [Google Scholar]
28. Zhang JY, Liu C, Zhou L, et al. A review of hydrogen as a new medical therapy. Hepato-Gastroenterology. 2012;59(116):1026?1032. doi:10.5754/hge11883 [PubMed] [CrossRef] [Google Scholar]
Articles from OncoTargets and therapy are provided here courtesy of Dove Press